Genomic approaches to asymptomatic chronic malaria
Head of the team
Dr. Antoine Claessens
Research interests
How Does Plasmodium falciparum Maintain Chronic, Asymptomatic Infections?
The GATAC-Malaria team is tackling this fundamental question by leveraging cutting-edge ‘Omics’ technologies and field-collected blood samples.
The Hidden Reservoir: A Challenge and an Opportunity
Asymptomatic Plasmodium falciparum infections are a major obstacle to malaria elimination efforts. These silent carriers not only sustain transmission but also provide a unique window into the long-term host-parasite interaction.
Our research focuses on understanding how P. falciparum survives and thrives during the 6-month dry season, when mosquito transmission is minimal. By studying blood samples from asymptomatic individuals in The Gambia, Cameroon, and Ghana, we aim to uncover the molecular strategies that enable the parasite to persist in human hosts.
Our Approach: Connecting Fieldwork to Molecular Insights
We employ advanced transcriptomics and genomics techniques, including:
- PacBio long-read sequencing
- Single-cell DNA sequencing
- Bulk RNAseq
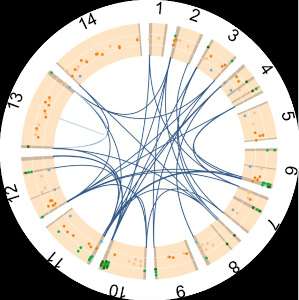
Our primary focus is on var gene transcription patterns, which drive antigenic variation—a key mechanism enabling the parasite to evade the immune system. Unlike previous studies relying on in vitro models of the lab-adapted 3D7 strain, we investigate these processes directly in field isolates. This allows us to test and refine hypotheses about mutually exclusive var gene expression in real-world settings.
Why It Matters
By revealing how P. falciparum establishes and maintains asymptomatic infections, we aim to identify critical molecular drivers of chronicity. These insights are essential for developing new strategies to disrupt the hidden infectious reservoir and advance malaria eradication efforts.
Recent Highlights
We recently published our main aims in Trends in Parasitology, here is a 2min video summary.
Our Collaborations and Funding
Our FRM team is part of ParaFrap, a consortium of French molecular parasitologists, and MalariaGEN, a consortium for malaria genomics. We are currently funded by FRM, ANR and Muse.
RECRUITMENT: Please get in touch if you are interested in joining our vibrant team as a Master / PhD /Post-doc.